Female sexual health represents a complex interplay of biological, psychological, and social factors that impact sexual function, satisfaction, and overall wellbeing. The evidence demonstrates that female sexual health is influenced by multiple determinants ranging from hormonal balance to psychological state, relational factors, and various medical conditions. This comprehensive report examines the underlying mechanisms of female sexual health, explores the various pathways through which it can be disrupted, and evaluates interventions based on their level of evidence and effectiveness.
The Multidimensional Nature of Female Sexual Health
Defining Sexual Health and Dysfunction in Women
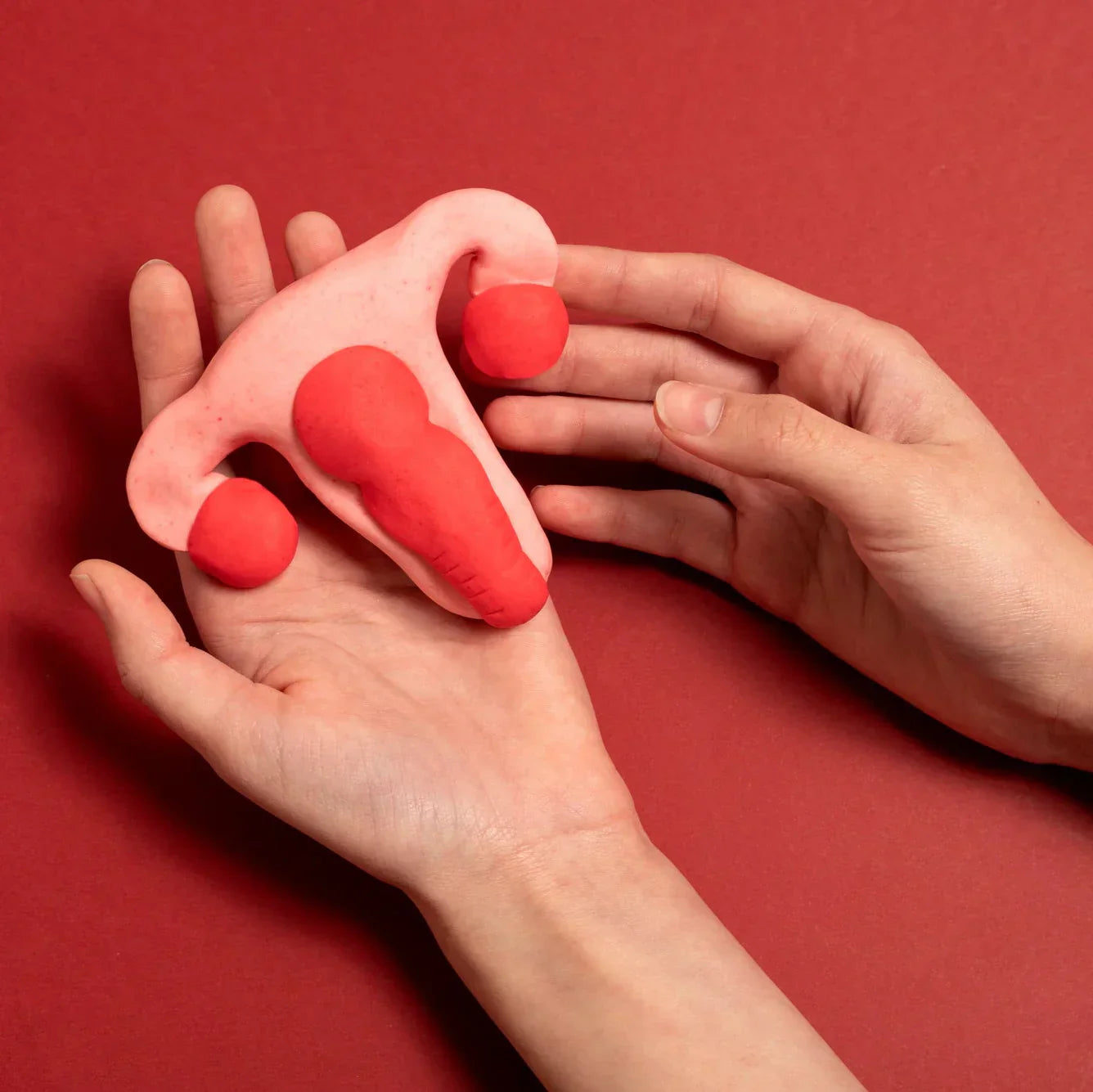
Female sexual health encompasses physical, emotional, mental, and social well-being in relation to sexuality. It is not merely the absence of disease or dysfunction but a positive and respectful approach to sexuality and sexual relationships. Female sexual dysfunction (FSD) represents a significant public health concern that affects women across the lifespan, manifesting as disorders of sexual desire, arousal, orgasm, or pain during sexual activity13. The assessment of female sexual function typically relies on validated instruments such as the Female Sexual Function Index, which measures various domains of sexual function including desire, arousal, lubrication, orgasm, satisfaction, and pain2. Sexual health is increasingly recognized as an essential component of overall health and quality of life, with sexual function being an important indicator of general wellbeing. The World Health Organization's holistic definition emphasizes that sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination, and violence.
Biopsychosocial Framework of Female Sexual Health
Female sexual health operates within a biopsychosocial framework where biological, psychological, and social factors continuously interact and influence one another. Biological factors include hormonal balance, vascular health, neurological function, and anatomical integrity. Psychological factors encompass mental health, body image, self-esteem, and past experiences. Social determinants include relationship quality, cultural norms, societal expectations, and access to healthcare1. This complex interplay means that disruption in any of these domains can impact sexual function and satisfaction. For example, research indicates that mood disorders can affect sexual desire and response, while relationship difficulties may contribute to decreased sexual satisfaction regardless of physical function18. The biopsychosocial model provides a comprehensive framework for understanding female sexual health that transcends purely medical perspectives and acknowledges the multifactorial nature of sexual wellbeing. This model is particularly important when addressing female sexual dysfunction, as effective interventions often need to target multiple domains simultaneously.
Biological Mechanisms Underlying Female Sexual Function
Hormonal Regulation and Endocrine Pathways
Hormonal balance plays a critical role in regulating female sexual function through multiple endocrine pathways. Estrogen supports vaginal tissue integrity, blood flow, and lubrication, while progesterone and androgens (particularly testosterone) influence sexual desire and arousal18. During menopause, declining estrogen levels lead to genitourinary syndrome of menopause, characterized by vaginal dryness, irritation, and dyspareunia (painful intercourse), significantly impacting sexual function1. Beyond sex hormones, thyroid function also substantially influences female sexual health. Research has identified thyroid hormone receptors in the genitourinary system, and both hypothyroidism and hyperthyroidism can disrupt sexual function through direct hormonal effects, neurotransmitter imbalances, and systemic consequences such as fatigue and mood disturbances8. The hypothalamic-pituitary-adrenal axis further modulates sexual function, with stress hormones like cortisol potentially suppressing sexual response when chronically elevated. This complex endocrine orchestra requires balance for optimal sexual function, with disruptions at any level potentially manifesting as sexual difficulties.
Vascular and Neurological Mechanisms
The sexual response cycle depends heavily on adequate blood flow to genital tissues and proper neurological signaling. Vascular health is essential for genital engorgement during arousal, with endothelial dysfunction potentially compromising this process1. Chronic low-grade inflammation associated with conditions like obesity can lead to endothelial dysfunction and compromised blood flow through the genitourinary system, directly affecting sexual arousal and response1. Neurologically, sexual function relies on an intricate network of autonomic and somatic nerves that facilitate arousal, orgasm, and pleasure sensations. Neurotransmitters including dopamine (promoting sexual interest), serotonin (with complex effects on arousal and orgasm), and norepinephrine (supporting arousal) all contribute to sexual response8. Nitric oxide plays a crucial role as a vasodilator that increases genital blood flow during sexual arousal, with reduced nitric oxide release associated with arousal difficulties8. Disruptions to these neurovascular pathways through medical conditions, medications, or surgical interventions can significantly impact sexual function, highlighting the importance of preserving neurovascular integrity during pelvic surgeries such as radical cystectomy for bladder cancer10.
Metabolic Influences on Sexual Function
Metabolic health exerts significant influence on female sexual function through several interconnected pathways. Insulin resistance, frequently associated with obesity and metabolic syndrome, can disrupt sexual function through vascular changes, hormonal imbalances, and inflammatory processes1. Obesity itself is associated with female sexual dysfunction through multiple mechanisms, including altered sex hormone metabolism, increased inflammatory markers, vascular changes, and psychological factors like poor body image13. While the relationship between obesity and female sexual function is not entirely consistent across studies, the preponderance of evidence suggests that higher BMI is associated with reduced sexual function and satisfaction3. Metabolic dysfunction can create a vicious cycle where hormonal imbalances affect sexual function, which in turn may impact psychological wellbeing and contribute to further metabolic disturbances. Understanding these complex metabolic pathways provides opportunities for intervention, as improvements in metabolic health through weight loss and physical activity have been shown to positively impact sexual function in many women13.
Factors Affecting Female Sexual Health
Medical Conditions and Their Impact
Various medical conditions significantly influence female sexual health through direct and indirect pathways. Endocrine disorders, including thyroid dysfunction, can disrupt sexual function through hormonal imbalances, neurotransmitter disturbances, and systemic effects813. Cancer and its treatments present particular challenges to sexual health, with surgical interventions, chemotherapy, radiotherapy, and hormonal therapies potentially causing anatomical alterations, nerve damage, vascular changes, and hormonal disruptions that impact sexual function515. Studies show that adverse sexual effects resulting from cancer treatments may affect more than half of women with cancer15. Genitourinary conditions such as vulvodynia (chronic vulvar pain) can cause significant sexual pain and dysfunction, with complex underlying mechanisms that may include neuroinflammation, pelvic floor dysfunction, and central sensitization14. Infectious diseases such as COVID-19 have also been linked to sexual health concerns, though the evidence remains preliminary and sometimes contradictory2. The interconnection between medical conditions and sexual function underscores the importance of considering sexual health as an integral component of comprehensive healthcare, rather than an isolated or secondary concern.
Psychological and Social Determinants
Psychological and social factors profoundly influence female sexual health and function. Mood disorders including depression and anxiety are strongly associated with sexual difficulties, affecting desire, arousal, and satisfaction18. Body image concerns, particularly prevalent among women with obesity or those who have undergone body-altering treatments such as mastectomy, can significantly impact sexual confidence and function1. Self-esteem and life satisfaction more broadly correlate with sexual wellbeing, with bidirectional effects where sexual satisfaction can enhance overall life satisfaction and vice versa1. Relationship factors, including partner's health, communication quality, and emotional intimacy, substantially influence sexual satisfaction. Social stigma surrounding female sexuality, body size, or sexual orientation can create additional barriers to sexual wellbeing1. Research indicates that sexual minority women (lesbian, bisexual) face unique challenges including higher rates of childhood sexual abuse and associated mental health concerns that may impact sexual function16. The intersection of these psychological and social factors creates a complex landscape where interventions often need to address multiple domains simultaneously to be effective.
Lifecycle Transitions and Hormonal Changes
Female sexual health undergoes significant transitions throughout the lifecycle, with particular challenges arising during major hormonal shifts. Menopause represents a critical cardiometabolic transition marked by estrogen decline, often accompanied by weight gain and redistribution of body fat, which can exacerbate sexual difficulties1. The genitourinary syndrome of menopause affects up to 50% of postmenopausal women, with symptoms including vaginal dryness, irritation, and dyspareunia directly impacting sexual comfort and satisfaction17. Pregnancy, childbirth, and the postpartum period present another significant transition, with hormonal fluctuations, physical changes, and new psychosocial dynamics potentially affecting sexual function. Adolescence and the onset of sexual activity introduce different challenges related to developing sexual identity, navigating relationships, and accessing appropriate healthcare. Each lifecycle transition presents both challenges and opportunities for intervention, with timely education and support potentially mitigating difficulties and enhancing sexual wellbeing. The recognition of these natural transitions is essential for normalizing related sexual changes while still addressing dysfunctions that significantly impact quality of life.
Evidence-Based Interventions for Female Sexual Health
Lifestyle Modifications and Weight Management
Lifestyle interventions show promising evidence for improving female sexual health, particularly for women with obesity or metabolic disturbances. Physical activity improves sexual function through multiple mechanisms including enhanced cardiovascular fitness, improved body image, reduced stress, and better mood regulation1. Dietary interventions focusing on anti-inflammatory and heart-healthy eating patterns may benefit sexual function by improving vascular health and reducing inflammatory markers1. Weight loss, whether achieved through lifestyle modification or bariatric surgery, has been associated with improved sexual function in the short term, though long-term outcomes require further investigation13. Studies demonstrate that lifestyle changes resulting in weight loss lead to better sexual function, and bariatric surgery has been shown to improve sexual function in the first couple of years following the procedure, yet the sustained effects beyond this timeframe remain uncertain3. The mechanisms behind these improvements likely include both physiological changes (improved hormonal profiles, reduced inflammation, better vascular function) and psychological benefits (enhanced body image, increased self-confidence). The accessibility and non-invasive nature of lifestyle interventions makes them an attractive first-line approach for many women experiencing sexual difficulties related to metabolic health.
Hormonal and Medical Treatments
Hormonal and medical treatments represent important interventions for addressing specific underlying causes of female sexual dysfunction. Hormone replacement therapy, particularly local estrogen treatment for postmenopausal women, effectively addresses vaginal dryness and pain during intercourse by restoring vaginal tissue integrity and lubrication1. Management of endocrine disorders such as thyroid dysfunction can significantly improve sexual function by normalizing hormonal imbalances and alleviating systemic symptoms that interfere with sexual wellbeing813. For women experiencing sexual difficulties related to specific medical conditions, treating the underlying condition often improves sexual function. For instance, appropriate management of vulvodynia using a combination of medical approaches (topical treatments, oral medications) can reduce pain and improve sexual comfort14. Medications specifically targeting female sexual dysfunction, such as flibanserin for hypoactive sexual desire disorder, have shown modest efficacy in selected populations, though their overall benefit-risk profile continues to be evaluated9. The effectiveness of hormonal and medical treatments highlights the importance of thorough diagnostic evaluation to identify specific underlying mechanisms that can be targeted with appropriate therapy, rather than taking a one-size-fits-all approach to female sexual dysfunction.
Psychological and Psychosexual Approaches
Psychological and psychosexual interventions demonstrate strong evidence for addressing female sexual difficulties across various populations. Cognitive-behavioral therapy (CBT) effectively addresses negative thought patterns, anxiety, and maladaptive behaviors that contribute to sexual dysfunction4. Mindfulness-based interventions help women develop present-moment awareness during sexual activity, reducing distraction and anxiety while enhancing sensation and pleasure. Relationship therapy addresses interpersonal factors that influence sexual satisfaction, including communication, emotional intimacy, and conflict resolution1. Sex therapy specifically targets sexual knowledge, skills, and comfort through directed exercises and guided exploration. Online and mobile psychotherapeutic treatments show promise in increasing accessibility of these interventions, particularly for women who face barriers to in-person therapy4. For women affected by cancer, psychological interventions addressing body image concerns, anxiety about sexual activity, and grief over changes in sexual function have proven especially beneficial5. The effectiveness of psychological approaches underscores the importance of addressing cognitive, emotional, and relational factors in female sexual health, even when physical or medical factors are also present. Integrating psychological interventions with medical treatments often yields better outcomes than either approach alone.
Emerging Treatments and Areas Requiring Further Research
Technological and Device-Based Interventions
Emerging technological interventions represent an evolving frontier in female sexual health treatments, with varying levels of evidence. Energy-based devices such as the CO2 RE Fractional CO2 Laser show promise for treating vaginal and vulvar tissue changes associated with genitourinary syndrome of menopause, though long-term efficacy data continue to develop17. These treatments aim to stimulate collagen production, improve vaginal tissue elasticity, and enhance mucosal integrity, potentially addressing dryness and pain during intercourse. Other technological approaches include pelvic floor biofeedback devices that help women develop awareness and control of pelvic floor muscles, which can benefit women with vaginismus or other pain disorders. Mobile applications focused on sexual education, tracking, and skill development provide accessible resources for women seeking to enhance their sexual health knowledge and practices. While these technological interventions show promise, the quality and quantity of supporting evidence varies significantly, with many requiring larger, longer-term studies to establish their place in treatment algorithms. The rapid pace of technological development in this field necessitates ongoing critical evaluation of emerging devices and applications to ensure they deliver meaningful benefits without undue risks or costs.
Special Populations and Targeted Approaches
Research increasingly recognizes the importance of tailored approaches for specific populations with unique sexual health needs. Sexual minority women face distinct challenges including higher rates of mental health concerns, substance use, and childhood trauma that may impact sexual wellbeing1618. Women with cancer require specialized interventions addressing the specific effects of various cancer treatments on sexual function, with evidence supporting multidisciplinary approaches combining medical management, psychological support, and sexual rehabilitation515. Postmenopausal women benefit from comprehensive approaches addressing both physical changes (vaginal dryness, tissue atrophy) and psychological adjustments to changing sexuality19. Women with a history of sexual trauma require trauma-informed care that addresses both physical symptoms and underlying psychological responses to sexual activity16. The growing research on these special populations highlights the importance of cultural competence, sensitivity to diverse sexual orientations and gender identities, and recognition of how multiple factors may intersect to influence sexual health outcomes. While targeted approaches show promise, many special populations remain understudied, with significant gaps in evidence regarding optimal interventions for transgender women, women with disabilities, and women from diverse cultural backgrounds20.
Critical Evaluation of Research Quality and Gaps
Despite growing recognition of female sexual health's importance, significant research gaps persist that limit evidence-based practice. Many studies investigating the relationship between medical conditions (such as thyroid disorders or obesity) and female sexual function show inconsistent results or methodological limitations38. Research on long-term outcomes of interventions, particularly surgical or device-based treatments, remains limited, with most studies reporting only short-term results317. The complex, multifactorial nature of female sexual function presents challenges for research design, with many studies focusing narrowly on single mechanisms or interventions rather than comprehensive approaches13. Additionally, validated outcome measures may not capture all relevant aspects of sexual wellbeing, particularly subjective satisfaction and quality of life impacts. Research often underrepresents certain populations, including older women, sexual and gender minorities, and women from diverse cultural backgrounds20. Moving forward, high-quality research utilizing standardized outcome measures, longer follow-up periods, and more diverse study populations is needed to strengthen the evidence base. Despite these limitations, the growing body of research in female sexual health represents significant progress in understanding mechanisms, pathways, and effective interventions, providing a foundation for both clinical practice and future investigation.
Conclusion
Understanding female sexual health requires recognition of its complex, multifactorial nature spanning biological, psychological, and social domains. The evidence clearly supports a comprehensive approach to assessment and treatment that addresses hormonal, vascular, neurological, and psychological mechanisms. Lifestyle modifications, hormonal treatments, psychological interventions, and specific medical therapies all show evidence of effectiveness when appropriately matched to underlying mechanisms of dysfunction. Despite significant advances in understanding female sexual health, important research gaps remain, particularly regarding long-term outcomes of interventions and optimal approaches for diverse populations. Moving forward, continued research, clinical awareness, and open dialogue about female sexual health will be essential to developing and implementing evidence-based interventions that enhance women's sexual wellbeing and overall quality of life.
Citations:
- https://pubmed.ncbi.nlm.nih.gov/38251874/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10515670/
- https://pubmed.ncbi.nlm.nih.gov/38112599/
- https://www.semanticscholar.org/paper/bab52fbe0ff559f5c7ae947911dad3adca0d5102
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8268945/
- https://pubmed.ncbi.nlm.nih.gov/33665545/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7268732/
- https://pubmed.ncbi.nlm.nih.gov/38600719/
- https://www.semanticscholar.org/paper/e8c60edfc94b62c695967b94451af97e56079243
- https://pubmed.ncbi.nlm.nih.gov/35916011/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11040903/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8330752/
- https://pubmed.ncbi.nlm.nih.gov/32234976/
- https://pubmed.ncbi.nlm.nih.gov/39586778/
- https://pubmed.ncbi.nlm.nih.gov/27607852/
- https://pubmed.ncbi.nlm.nih.gov/37166921/
- https://www.semanticscholar.org/paper/d8681c83faf23bbdc9bce97d7c316b24304b2069
- https://pubmed.ncbi.nlm.nih.gov/37946724/
- https://pubmed.ncbi.nlm.nih.gov/30229521/
- https://pubmed.ncbi.nlm.nih.gov/39400250/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7065174/
- https://pubmed.ncbi.nlm.nih.gov/30565482/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10117494/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9096608/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3205538/
- https://www.semanticscholar.org/paper/a172e5170998f5c4d1bee8a3e420505a1338e10f
- https://pubmed.ncbi.nlm.nih.gov/38888098/
- https://pubmed.ncbi.nlm.nih.gov/34913798/
- https://pubmed.ncbi.nlm.nih.gov/12851124/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10422970/
- https://pubmed.ncbi.nlm.nih.gov/28644334/
- https://www.semanticscholar.org/paper/4f9277db14b5d3c9d9448cec87fd16995b378cae
- https://pubmed.ncbi.nlm.nih.gov/37540144/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8882295/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6167003/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8661283/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10583075/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8857844/
- https://www.semanticscholar.org/paper/bd4b517bd07009cba5f5d6a646e069b130931b58
- https://pubmed.ncbi.nlm.nih.gov/27455852/
- https://www.semanticscholar.org/paper/f9c755f4bab8659a7dd998abfc57a6ee742d4f97
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11077700/
- https://www.semanticscholar.org/paper/6142af9216442c124fc4998f783560f917c05fed
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9947888/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9806966/
- https://www.semanticscholar.org/paper/55fb113c3ddbe76e1e17e3a3fc7f5127f51120a5
- https://www.semanticscholar.org/paper/e3e4b936d25d17b39d2096e7cf3705f888e2eac6
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7617419/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7957010/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6773357/
- https://www.semanticscholar.org/paper/c035e602904fbcaf0e3ea523700bd57b2407cf17
- https://www.semanticscholar.org/paper/cf7cfb1ce3d434919034dfbd7c7c3a1585e06012
- https://www.semanticscholar.org/paper/1d1075f89d22d52dabd1f9e83cfc49ef50e57307
- https://pubmed.ncbi.nlm.nih.gov/39455741/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10136821/
- https://www.semanticscholar.org/paper/0cb8507fada336b6aeff9fe9b105f1328391880a
- https://www.semanticscholar.org/paper/88f936d95deff448d95253140bdb2f5ca274a918